This chemical binding and inactivation of mercury does take place. Mercury has a great affinity for selenium, estimated to be approximately one million times stronger than mercury’s affinity for sulfur. So, selenium’s binding with mercury in the tissues does keep the mercury from getting into mischief in the brain and spinal cord, peripheral nervous system, and endocrine system.
Mercury and selenium: understood the other way around
However, the real mischief that mercury gets up to is that it inhibits the body’s ability to make the antioxidant selenoproteins that are needed to protect against oxidative damage in the brain and neuroendocrine tissues.
Mercury does this by binding up the selenium in selenocysteine, the 21st amino acid, that would otherwise be available for the formation of selenoproteins. In effect, mercury holds selenium prisoner and keeps it from its antioxidant functions.
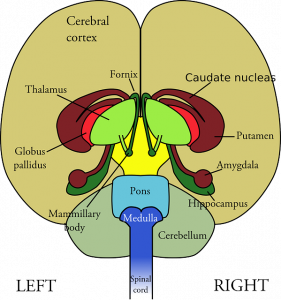
The brain is especially susceptible to oxidative damage caused by reactive oxygen species (free radicals) because the brain uses approximately 20% of the oxygen consumed by the body to establish and maintain its millions of neuronal connections.
- In using oxygen, the brain deliberately creates free radicals to transmit redox signals.*
- When all goes well, the redox signaling regulates critical functions in the brain and nervous system.
- Whenever there is an overproduction of free radicals, however, and an imbalance between free radicals and antioxidants, then the brain cells and tissues suffer oxidative damage.
* Please note: It is a common misconception that reactive oxygen species act only as harmful free radicals causing oxidative damage. The central role of reactive oxygen species in cell signaling needs to be recognized. It is the imbalance of free radicals and antioxidants that causes oxidative damage.
Professor Nicholas Ralston and Dr. Laura J. Raymond explain in a recent review article that the toxic effect on the brain and nervous system comes primarily from mercury’s inhibition of selenium metabolism. Selenium metabolism is inhibited because the mercury binds with and sequesters the selenium and depletes the body’s stores of selenium for the formation of selenoproteins. The toxic effect on the brain comes about, then, because there is inadequate antioxidant protection [Ralston & Raymond, 2018].
The brain especially vulnerable to oxidative damage
The brain is particularly vulnerable to oxidative damage in the absence of adequate antioxidant selenoprotein protection for a variety of reasons [Ralston & Raymond 2018]:
- The brain has limited antioxidant enzyme pathways, which are abundantly available in other tissues.
- The brain has high iron content, which could potentiate oxidative damage.
- The brain has an abundance of long chain polyunsaturated fatty acids, which are vulnerable to lipid oxidation.
Mercury’s disruption of selenium biochemistry
The title of Professor Ralston and Dr. Raymond’s 2018 journal article is revealing: Mercury’s neurotoxicity is characterized by its disruption of selenium biochemistry.
Their thesis is that it is the loss of cellular redox control that causes much of the mercury-related damage to the brain and neuroendocrine system. Under normal conditions, the production and removal of reactive oxygen species and reactive nitrogen species maintains the proper functioning of the cellular redox signaling proteins. That proper functioning is necessary for cell survival. An imbalance of reactive oxygen species and antioxidants results in oxidative stress and oxidative damage [Ralston & Raymond 2018].
Lack of adequate selenium status to produce selenium containing antioxidant selenoproteins is a cause of the loss of cellular redox control. Loss of cellular redox control results in oxidative stress and damage to brain cells and tissues.
Selenium: the biochemical target of mercury
Dr. Ralston and Dr. Raymond believe that selenium itself is the biochemical target of the toxic methylmercury molecules. Once methylmercury enters the body, it is channeled into metabolic pathways where it disrupts or interrupts normal necessary selenium metabolism.
The “protective effect” of selenium
In other words, it is convenient but imprecise and misleading to talk solely about a “protective” effect of selenium in the context of mercury toxicity. That explanation does not go far enough.
It is not just that selenium is counteracting and protecting against mercury toxicity per se. Rather, it is the case that the damage to the brain and nervous system that is associated with mercury toxicity is typical of the oxidative damage that results from a depletion of antioxidant selenoenzymes.
Professor Ralston and Dr. Raymond say that the damage from selenium deficiency – the oxidative damage – results in most of the characteristics that we associate with mercury toxicity. Thus, mercury’s harmful effects seem to arise primarily from the inhibition of selenium metabolism. If there is sufficient selenium available to support the selenoenzyme activities in the brain, then the harmful effects of toxic doses of mercury will not develop [Ralston & Raymond 2018].
- There can be a prolonged delay between the ingestion of a harmful dose of mercury and the onset of symptoms. The severity of the brain damage caused by mercury exposure is directly associated with the dose, but the latency period is not.
- The latency period varies according to the selenium status of the victim of mercury exposure.
- Mercury exposures in the absence of adequate selenium status follow a similar sequence of symptoms:
- tingling sensation in the lips and extremities
- loss of motor coordination
- difficulty pronouncing words
- vision constriction
- deafness
- death in the case of lethal dosages
Importance of successful selenium metabolism
Successful selenium metabolism is important because elemental selenium, incorporated into the amino acid selenocysteine, is a key component of the 25 known selenoproteins found in humans. Many of these selenoproteins are selenoenzymes that are need to prevent and reverse oxidative damage in the brain and neuroendocrine system.
- the glutathione peroxidases (especially GPx 1, 2, 4, and 6)
- The thioredoxin reductases (TXNRD 1-3)
- the selenoproteins M, N, and W
The formation of these selenoenzymes is especially vulnerable to irreversible disruption and inhibition by methylmercury. The disruption and interruption of the selenoenzymes’ antioxidant activity is what appears to cause many of the pathological effects of mercury toxicity [Ralston & Raymond 2018].
The importance of the antioxidant selenoenzymes is seen in the body’s preferential delivery and preservation of these selenoproteins to the brain and neuroendocrine tissues in times of inadequate selenium status [Ralston & Raymond].
Exposure to mercury and the blood-brain barrier
Low-level exposure to mercury and methylmercury is common and generally without adverse effects. High levels of exposure, however, are neurotoxic because mercury and methylmercury readily cross the blood-brain barrier, and, in the brain and the nervous system, they preferentially bind with selenium, robbing these organs of the needed selenium [Ralston & Raymond, 2018].
Exposure to mercury and the placental blood barrier
The placental barrier is very weak at blocking the passage of toxic chemicals. It does not block the passage of methylmercury compounds from mother to fetus.
Moreover, the fetus generally lacks a reserve of tissue selenium. If there is a loss of maternal selenium supply to the fetus because the mother’s selenium is increasingly bound up with toxic mercury, then there will be impaired selenium metabolism in the fetal brain with dire consequences for fetal brain development [Ralston & Raymond 2018].
The review of available research indicates that pregnant women who eat “safe” ocean fish containing selenium in molar excess of mercury give birth to children with improved neurological development. Pregnant women who avoid eating “safe” ocean fish during pregnancy may give birth to children at significant risk for health and development problems [Ralston & Raymond 2018].
Dietary sources of selenium
Professor Ralston and Dr. Raymond say that ocean and freshwater fish are the dominant source of dietary exposures to methylmercury.
However, studies show that many ocean fish have molar ratios of selenium and mercury in favor of selenium and thus may be considered “safe” to eat. The ocean fish with unfavorable selenium-mercury molar ratios should be avoided [Ralston & Raymond 2018]:
- Predatory whales
- Sharks
- Swordfish
- Halibut
With respect to fresh-water fish and farm fish, the selenium-mercury molar ratios may vary according to the regional content of selenium in the soil. It is best to check for local reports of selenium-mercury molar ratios and to check the http://www.seafoodwatch.org/ website.
Conclusions about mercury and selenium biochemistry
Selenium and selenoproteins are important to good brain and neuroendocrine system health. During periods of extended selenium deficiency, the selenium content of such organs as the liver, the muscle, and the blood will decline so that the brain and endocrine tissues can remain supplied [Ralston & Raymond 2018].
High concentrations of mercury in the brain and endocrine tissues appear to be without toxicity consequences as long as there remains some selenium free from binding with mercury so that the synthesis of the vital antioxidant selenoenzymes can take place [Ralston & Raymond 2018].
The importance of selenium supplementation in regions in which dietary intakes of selenium are inadequate can be seen in recent studies that have shown that selenium-enriched diets not only prevent methylmercury toxicity but can also reverse some of the most severe symptoms associated with mercury poisoning [Ralston & Raymond 2018].
Sources
Ralston, N. V. C. & Raymond, L. J. (2018). Mercury’s neurotoxicity is characterized by its disruption of selenium biochemistry. Biochim Biophys Acta, pii: S0304-4165(18)30141-7. doi: 10.1016/j.bbagen.2018.05.009. [Epub ahead of print]
Richie, J. J., Das, A., Calcagnotto, A. M., Sinha, R., Neidig, W., Liao, J., & … El-Bayoumy, K. (2014). Comparative effects of two different forms of selenium on oxidative stress biomarkers in healthy men: a randomized clinical trial. Cancer Prevention Research (Philadelphia, Pa.), 7(8), 796-804. doi:10.1158/1940-6207.CAPR-14-0042
The information presented in this review article is not intended as medical advice and should not be construed as such.
