Researchers at the University of Arizona in Tucson, home of the Arizona Cancer Center, identified a statistically significant direct relationship between selenium and Type-2 diabetes in observational studies but no statistically significant relationship in randomized controlled trials [Kohler 2018].
Note: Randomized controlled trials are the gold standard for scientific evidence in the bio-medical field. The randomization of the study participants should produce comparable groups and should eliminate accidental bias. In observational studies, the researchers do not randomly assign the study participants to groups and do not decide which treatments each group receives or does not receive.
The differences between the findings in observational studies and in randomized controlled trials could be explained by the role of as-yet-unexplained uncontrolled confounding variables in the observational studies. There may be a third factor that affects both selenium status and the risk of type-2 diabetes that is not adequately controlled in the observational studies [Jacobs 2019].
Evidence from Three Clinical Trials of Selenium Supplementation
The University of Arizona researchers examined the data from three randomized clinical trials with a combined total of 20,290 participants [Kohler 2018]:
- Nutritional Prevention of Cancer Trial (n = 1202 men and women)
- Selenium and Vitamin E Cancer Prevention Trial (n = 17,448 men)
- Selenium Trial (n = 1640 men and women)
Those three clinical trials assessed cancer or precancerous lesions as a primary outcome.
In each trial, the study participants received 200 micrograms of selenium daily:
- Nutritional Prevention of Cancer Trial (natural selenized yeast)
- Selenium and Vitamin E Cancer Prevention Trial (synthetic selenomethionine)
- Selenium Trial (natural selenized yeast)
Secondary Analysis of Data from the Selenium Clinical Trials
Secondary analysis of the data from the Nutritional Prevention of Cancer Trial showed that there was a statistically significantly increased risk of type-2 diabetes only in the highest tertile of the study participants’ baseline plasma selenium levels: the study participants above 121.6 micrograms per liter [Stranges 2007].
On the other hand, the Selenium and Vitamin E Cancer Prevention Trial (SELECT) and the Selenium Trial showed no statistically significant overall increased risk for Type-2 diabetes risk after supplementation with 200 micrograms of selenium per day compared with placebo supplementation [Jacobs 2019].
Moreover, analysis of the data from a sub-set of 175 of the 400 individuals who participated in the Selenium Trial showed that the data do not support a significant adverse effect of daily selenium supplementation with 200 micrograms/day of selenized yeast on beta-cell function or insulin sensitivity. These findings provide important evidence that selenium supplementation for up to three years in older individuals does not result in diabetogenic effects in humans. Sub-group analysis of the data by age and sex did not change the outcome [Jacobs 2019].
Relationship between Baseline Plasma Selenium Level, Supplementation, and Increased Risk of Diabetes?
Two Norwegian case-control studies have shown no statistically significant relationship between selenium and type-2 diabetes [Simic 2017; Hansen 2017].
Kohler et al point out that the baseline blood selenium levels were considerably lower in the Norwegian study participants (median: 100-105 micrograms per liter) than in the three US randomized controlled trials [Kohler 2018]:
- Nutritional Prevention of Cancer Trial (median: 113 micrograms per liter)
- SELECT Trial (median: 135 micrograms per liter)
- Selenium Trial (median: 136 micrograms per liter)
Selenium Supplementation Reduces Fasting Insulin Levels, HOMA-IR Levels, and HOMA-beta Levels
Stróżyk et al analyzed the data from four randomized controlled trials enrolling 241 study participants. In these studies, the selenium supplementation significantly reduced the fasting insulin levels, the HOMA-IR levels, and the HOMA-beta levels [Stróżyk 2019].
Note: HOMA-IR and HOMA-beta are equations used to assess insulin resistance and pancreatic beta–cell function.
Mahdavi Gorabi et al reviewed 12 articles published between 2004 and 2016. The 12 studies were all randomized, double-blind, placebo-controlled studies. They comprised 757 participants randomly assigned to an intervention group and 684 participants assigned to a control group [Mahdavi Gorabi].
The aggregated data from the 12 studies showed that selenium supplementation resulted in a significant decrease in homeostasis model of assessment-estimated β-cell function(HOMA-B) and a significant increase in quantitative insulin sensitivity check index (QUICKI) as compared with the controls [Mahdavi Gorabi].
Otherwise, the data showed no statistically significant improvements in glycemic indices such as fasting plasma glucose, insulin, homeostasis model of assessment-estimated insulin resistance (HOMA-IR), Hemoglobin A1c (HbA1c), and adiponectin. The researchers concluded that the meta-analysis indicated that selenium supplementation significantly decreased HOMA-B and increased QUICKI score [Mahdavi Gorabi].
Summary of Evidence Related to Selenium Supplementation and Type-2 Diabetes Risk
- The relationship between selenium and selenoproteins and type-2 diabetes is undoubtedly complex. The mechanism for a possible cause-effect relationship between selenium exposure and type-2 diabetes risk is unknown [Rayman 2013].
- The scientific evidence is inconsistent and confusing. Observational studies seem to show a link between selenium supplementation and type-2 diabetes [Kim 2019]. However, the evidence comes more from observation studies done with selenium-replete Americans than from observational studies done with selenium-poor Europeans whose life-style differs from that of Americans [Steinbrenner 2011].
- Randomized controlled trials, on the whole, do not show any conclusive evidence of such a link [Kohler 2018, Jacobs 2019].
- Some researchers warn against widespread and indiscriminate use of selenium supplements by the general public [Rayman 2013]. It is best to have one’s serum selenium level tested before deciding which dosage to take. The current evidence seems to suggest that there may be a modest increase in the risk of type-2 diabetes with higher levels of selenium in the blood circulation or with selenium supplementation for chemo-prevention [Kohler 2018].
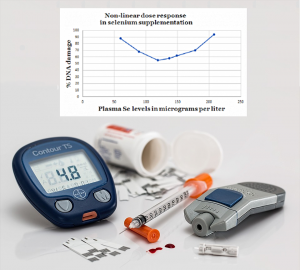
- Professor Margaret P. Rayman suggests a U-shaped relationship between serum selenium status and disease risk. In her depiction, a serum selenium level of 125 micrograms per liter is labeled “adequate.” She does not say how far below and above 125 micrograms/liter the significantly increased risk of disease begins [Rayman 2019].
- A study done in the UK has shown that a daily dietary intake of 55 micrograms of selenium combined with 50 or 100 micrograms in daily selenium supplements increases plasma selenium levels from a baseline of 95.7 micrograms per liter to just below and just above Professor Rayman’s “adequate” level [Hurst 2010]:
- To 118.3 micrograms per liter with a daily selenium supplement of 50 micrograms
- To 152.0 micrograms per liter with a daily selenium supplement of 100 micrograms
- No studies have been done to distinguish the effects of specific species of selenium on diabetogenic activity. These studies are needed [Vinceti 2018].
Sources
Hansen AF, Simic A, Asvold BO, Romundstad PR, Midthjell K, SyversenT, Flaten TP. (2017). Trace elements in early phase type 2 diabetes mellitus—a population-based study: the HUNT study in Norway. J Trace Elem MedBiol; 40:46–53.
Jacobs ET, Lance P, Mandarino LJ, Ellis NA. (2019). Selenium supplementation and insulin resistance in a randomized, clinical trial. BMJ Open Diabetes Res Care, e000613.
Kim J, Chung HS, Choi M-K, Roh YK, Yoo HJ, Park JH, Kim DS, Yu JM, Moon S. (2019). Association between serum selenium level and the presence of diabetes mellitus: a meta-analysis of observational studies. Diabetes Metab J, 43:e1.
Kohler LN, Foote J, Kelley CP, Florea A, et al. (2018). Selenium and type 2 diabetes: systematic review. Nutrients, 10(12): E1924.
Kohler LN, Florea A, Kelley CP, Chow S, Hsu P, Batai K, Saboda K, Lance P & Jacobs ET. (2018), Higher plasma selenium concentrations are associated with increased odds of prevalent type 2 diabetes. J. Nutr; 148(8): 1333-1340.
Mahdavi Gorabi A, Hasani M, Djalalinia S & Zarei M. (2019). Effect of selenium supplementation on glycemic indices: a meta-analysis of randomized controlled trials; J Diabetes Metab Disord 2019 18 349-362.
Rayman MP, Stranges S. (2013) Epidemiology of selenium and type-2 diabetes: can we make sense of it? Free Radic Biol Med, 65:1557–1564.
Rayman MP. (2019). Selenium intake, status, and health: a complex relationship. Hormones (Athens), https://doi.org/10.1007/s42000-019-00125-5.
Simic A, Hansen AF, Asvold BO, Romundstad PR, Midthjell K, SyversenT, Flaten TP. (2017). Trace element status in patients with type 2 diabetes in Norway: the HUNT3 survey. J Trace Elem Med Biol; 41:91–8.11.
Steinbrenner H, Speckmann B, Pinto A, Sies H. (2011). High selenium intake and increased diabetes risk: experimental evidence for interplay between selenium and carbohydrate metabolism. J Clin Biochem Nutr, 48: 40-5.
Stranges S, Marshall JR, Natarajan R, Donahue RP, et al. (2007). Effects of long-term selenium supplementation on the incidence of type 2 diabetes: a randomized trial.
Ann Intern Med, 147: 217-23.
Stróżyk A, Osica Z, Przybylak JD, Kołodziej M, Zalewski BM, Mrozikiewicz-Rakowska B, Szajewska H. (2019).
Effectiveness and safety of selenium supplementation for type 2 diabetes mellitus in adults: a systematic review of randomised controlled trials. J Hum Nutr Diet; 32(5):635-645.
Vinceti M, Filippini T, Del Giovane C, & Crespi CM. (2018). Selenium for preventing cancer. Cochrane Database Syst Rev. CD005195.
The information presented in this review article is not intended as medical advice and should not be used as such.
16 January 2020
