Heart failure – the inability of the heart muscle to pump a sufficient quantity of blood out to the body – is a debilitating disease, resulting in shortness of breath, congestion in the lungs, and pooling of blood in the lower extremities. Heart failure is equivalent to diminished quality of life.
The prognosis for heart failure is poor, and the available medical therapies for patients with heart failure are inadequate. New treatment strategies are needed [Mortensen 2015].
Yin et al have analyzed the data from 39,757 adults in a cross-sectional study from the 2005–2018 US National Health and Nutrition Examination Survey. Their findings suggest that high levels of combined dietary antioxidant micronutrients are associated with decreased prevalence of various forms of cardiovascular disease and that selenium has the greatest contribution to this association [Yin 2022].
Nils Bomer and a group of cardiologists in The Netherlands, Scotland, and England have suggested that cardiologists pay close attention to heart failure patients’ status with respect to the micronutrients selenium, Coenzyme Q10, zinc, iron, and copper and consider supplementation as a useful therapeutic strategy for the treatment of heart failure patients [Bomer 2022].
Sub-Optimal Selenium, Coenzyme Q10, Zinc, Iron, and Copper Status in Heart Failure Patients
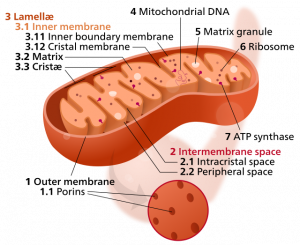
The mitochondrial electron transport chain needs selenium, Coenzyme Q10, zinc, iron, and copper for efficient ATP energy production and for antioxidant defense against the effects of harmful free radicals. Heart failure patients are known to have low intakes of selenium, zinc, and iron; moreover, heart failure patients are known to synthesize less Coenzyme Q10 than healthy individuals do [Bomer 2022].
Deficient or sub-optimal status of these micronutrients may contribute to
defective mitochondrial function, diminished antioxidant protection, and reduced capacity for ATP energy generation in heart failure patients [Bomer 2022].
Selenium and heart health
Selenium is needed as a component of the amino acid selenocysteine. Selenocysteine is needed as a component of the selenoproteins, the glutathione peroxidases and the thioredoxin reductases. These selenoproteins function as antioxidant enzymes to prevent the harmful accumulation the harmful free radical hydrogen peroxide inside the cells and the mitochondria [Bomer 2022].
In a cohort study, researchers found that serum selenium status below 100 mcg/L in heart failure patients is significantly associated with reduced exercise capacity and higher mortality, which suggests that serum selenium concentrations below 100 mcg/L might constitute deficiency status [Bomer 2020].
In the randomized controlled trial, the KiSel-10 Study, Prof. Urban Alehagen and a team of researchers administered selenium and Coenzyme Q10 supplements or placebo to elderly community living citizens aged 70-88 years. The mean serum selenium level of the study participants was quite low: 67.1 mcg/L [Alehagen 2013; Alehagen 2020].
The combined supplementation with 1 x 200 mcg/day of selenium and 2 x 100 mg of Coenzyme Q10 for four years was associated with significantly lower risk of death from heart disease and with significantly better heart function as seen on echocardiograms, compared to placebo [Alehagen 2013]. The beneficial heart health effects persisted after cessation of the combined supplementation for another eight years [Alehagen 2018].
Coenzyme Q10 and heart health
The primary source of Coenzyme Q10 is endogenous bio-synthesis. The human adult bio-synthesis of Coenzyme Q10 declines with increasing age [Kalén 1989]. Supplementation is necessary to make up for the reduced bio-synthesis. In heart failure patients, lower plasma CoQ10 concentrations
are associated with poorer New York Heart Association functional class, lower left ventricular ejection fraction, and higher plasma concentrations
of NT-proBNP, a known blood bio-marker for heart failure [Bomer 2022].
Coenzyme Q10 plays key role in the production of ATP in the mitochondria. In addition, CoQ10 inhibits the peroxidation of lipids and lipoproteins and protects cell membranes against oxidation. The oxidative stress that comes with heart failure may deplete CoQ10 status [Bomer 2022].
We have mentioned the use of CoQ10 supplementation in the KiSel-10 Study. In the randomized controlled trial, the Q-Symbio Study, Dr. Svend Aage Mortensen and a team of researchers administered Coenzyme Q10 3 x 100 mg/day or similar placebos to chronic heart failure patients for two years. The CoQ10 supplementation was significantly associated with reduced need for hospitalization for worsening heart failure, reduced incidence of cardiovascular death, reduced need for mechanical assist implantation or urgent cardiac transplantation, compared with placebo. In addition, the CoQ10 supplementation was significantly associated with a reduction in all-cause mortality [Mortensen 2014].
Similarly, in the Morisco study, the researchers administered 2 mg Coenzyme Q10 per kilogram of body weight or placebo per day in a 12-month randomized controlled trial. The heart failure patients receiving the active treatment reported significantly fewer heart failure-related hospitalizations and complications than the heart failure patients in the placebo group [Morisco 1993].
Zinc and heart health
Bomer et al [2022] note that zinc deficiency in heart failure patients may be caused by low dietary intake common in many regions of the world, by reduced gastrointestinal absorption, and/or by increased excretion as the result of neurohormonal activation. Medications to lower blood pressure such as ACE inhibitors and angiotensin II receptor blockers increase zinc excretion.
Zinc is an important component of the endogenous superoxide dismutase antioxidant enzyme. When the production of harmful free radicals in the mitochondria exceeds the antioxidant activity of superoxide dismutase, there is increased cell degeneration and, eventually, cell death [Bomer 2022].
Observational studies have shown that serum zinc concentrations are lower in heart failure patients than in healthy volunteers and that serum zinc concentrations less than 75 mcg/dl in heart failure patients are associated with a higher cardiovascular mortality and higher all-cause mortality [Bomer 2022]. There is a need for clinical trials of enrolling heart failure patients with zinc deficiency to test the therapeutic role of zinc supplementation.
Iron and heart health
Bomer et al [2022] state that iron deficiency is associated with hypoxia, i.e., insufficient delivery of oxygen to the tissues and organs, resulting in mitochondrial dysfunction, reduced ATP production and impaired
contraction and relaxation of the heart muscle. However, an excess of unbound iron in the mitochondria can also lead to the production of harmful free radicals that, unchecked, damage the mitochondria and other organelles in the cells. In the mitochondria, most of the iron needs to be bound to ferritin [Bomer 2022].
Iron deficiency is a common nutritional disorder, and clinical studies show that IV iron supplementation of heart failure patients is associated with beneficial effects on the symptoms, quality of life, and exercise capacity of the patients. Oral iron supplementation has not given the same beneficial outcomes. Thus, it is recommended that all heart failure patients be tested for iron deficiency and treated with IV iron as necessary [Bomer 2022].
Copper and heart health
Bomer et al [2022] have found no evidence to support copper supplementation. In general, they warn that studies show higher blood concentrations of copper found in patients with heart failure than in healthy control individuals. One study has found that patients who died or were hospitalized for heart failure had, on average, a higher serum copper concentration than those who did not die or need to be hospitalized.
A meta-analysis of data from 13 studies enrolling 1504 study participants showed an association between heart failure and high serum copper
concentrations.
Diets Adequate in Macronutrients But Not in Micronutrients
In analyzing the reason that the heart muscle begins to generate too little ATP energy, Bomer et al realized that the problem is not with the dietary supply of macronutrients such as fatty acids, lactic acid, and carbohydrates. The typical diet provides adequate quantities of these fuels for ATP energy generation.
Instead, what is often lacking is an adequate supply of the micronutrients – selenium, Coenzyme Q10, zinc, and iron. These micronutrients are needed in sufficient quantities to enable the mitochondrial production of ATP energy and to provide antioxidant protection against the harmful free radicals that are created during the process of ATP energy production.
The reduction in the bio-energetic capacity caused by sub-optimal supply of these micronutrients can play a major role in the development and worsening of heart failure, according to Bomer [2022].
Conclusion: Heart Muscle Defective Because of Micronutrient Deficiencies
Bomer et al address the issue of a failing heart muscle that seems to be “out of fuel.”
They conclude that it will not help much to provide more fuel in the form of fatty acids, glucose, and ketones to the heart muscle if the mitochondria in the heart muscle do not have enough micronutrients to turn the fatty acids, glucose, and ketones into ATP energy without doing excessive oxidative damage to the heart muscle [Bomer 2022].
When there are deficiencies of selenium and Coenzyme Q10, in particular, the heart muscle is vulnerable to damage caused by harmful free radicals that are a by-product of the process or ATP energy generation [Bomer 2022].
Micronutrient deficiencies, they say, change the paradigm from a heart muscle out of fuel to a heart muscle that is defective and “on a path to self-destruction” [Bomer 2022].
Sources
Alehagen U, Johansson P, Björnstedt M, Rosén A, Dahlström U. Cardiovascular mortality and N-terminal-proBNP reduced after combined selenium and coenzyme Q10 supplementation: a 5-year prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. Int J Cardiol. 2013 Sep 1;167(5):1860-6.
Alehagen U, Aaseth J, Alexander J, Johansson P. Still reduced cardiovascular mortality 12 years after supplementation with selenium and coenzyme Q10 for four years: A validation of previous 10-year follow-up results of a prospective randomized double-blind placebo-controlled trial in elderly. PLoS One. 2018;13(4):e0193120.
Alehagen U, Aaseth J, Alexander J, Johansson P, Larsson A. Supplemental selenium and coenzyme Q10 reduce glycation along with cardiovascular mortality in an elderly population with low selenium status – A four-year, prospective, randomised, double-blind placebo-controlled trial. J Trace Elem Med Biol. 2020 May 4;61:126541.
Bomer N, Pavez-Giani MG, Grote Beverborg N, Cleland JGF, van Veldhuisen DJ, van der Meer P. Micronutrient deficiencies in heart failure: Mitochondrial dysfunction as a common pathophysiological mechanism? J Intern Med. 2022 Feb 9. Epub ahead of print.
Bomer N, Grote Beverborg N, Hoes MF, Streng KW, Vermeer M, Dokter MM, IJmker J, Anker SD, Cleland JGF, Hillege HL, Lang CC, Ng LL, Samani NJ, Tromp J, van Veldhuisen DJ, Touw DJ, Voors AA, van der Meer P. Selenium and outcome in heart failure. Eur J Heart Fail. 2020 Aug;22(8):1415-1423.
Girerd N. Is the correction of micronutrient deficiencies the next step in heart failure management? J. Intern Med. 2022 Feb 9. Epub ahead of print.
Kalén A, Appelkvist EL, Dallner G. Age-related changes in the lipid compositions of rat and human tissues. Lipids. 1989 Jul;24(7):579-84.
Morisco C, Trimarco B, Condorelli M. Effect of coenzyme Q10 therapy in patients with congestive heart failure: a long-term multicenter randomized study. Clin Investig. 1993;71(8 Suppl):S134-6.
Mortensen SA, Rosenfeldt F, Kumar A, Dolliner P, Filipiak KJ, Pella D, Alehagen U, Steurer G, Littarru GP; Q-SYMBIO Study Investigators. The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC Heart Fail. 2014 Dec;2(6):641-9.
Mortensen, S. A. Coenzyme Q10: will this natural substance become a guideline-directed adjunctive therapy in heart failure? JACC. Heart Failure. 2015;3(3):270-271.
Yin T, Zhu X, Xu D, Lin H, Lu X, Tang Y, Shi M, Yao W, Zhou Y, Zhang H and Li X. The Association between dietary antioxidant micronutrients and cardiovascular disease in adults in the United States: A cross-Sectional
study. Front. Nutr. 2022;8:799095.
15 March 2022
The information presented in this review article is not intended as medical advice and should not be used as such.
